Connect With Us
Blog

Biomechanical Impact of Wearing High Heels

High heels significantly impact walking, with notable effects on gait, biomechanics, and control. Wearing high heels can alter the way people walk in several ways, presenting valuable insights for both designers and podiatrists. The primary changes observed in high-heel walking encompass alterations in the foot's rollover function, modifications in ankle and knee joint dynamics, and shifts in lower back posture, accompanied by compromised step length and balance. The heightened heel height forces the foot into an increased plantar flexion, which, in turn, augments knee flexion and causes an increased curvature of the lower back. Understanding the biomechanical adjustments associated with high heel-wearing is vital for designing more comfortable and less detrimental footwear, in addition to addressing potential musculoskeletal issues arising from prolonged use. If you enjoy wearing high heels and want to continue wearing them while paying attention to your feet and body, it is suggested that you schedule an appointment with a podiatrist to discuss this topic further.
High heels have a history of causing foot and ankle problems. If you have any concerns about your feet or ankles, contact Elie C. Daniel, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Effects of High Heels on the Feet
High heels are popular shoes among women because of their many styles and societal appeal. Despite this, high heels can still cause many health problems if worn too frequently.
Which Parts of My Body Will Be Affected by High Heels?
- Ankle Joints
- Achilles Tendon – May shorten and stiffen with prolonged wear
- Balls of the Feet
- Knees – Heels cause the knees to bend constantly, creating stress on them
- Back – They decrease the spine’s ability to absorb shock, which may lead to back pain. The vertebrae of the lower back may compress.
What Kinds of Foot Problems Can Develop from Wearing High Heels?
- Corns
- Calluses
- Hammertoe
- Bunions
- Morton’s Neuroma
- Plantar Fasciitis
How Can I Still Wear High Heels and Maintain Foot Health?
If you want to wear high heeled shoes, make sure that you are not wearing them every day, as this will help prevent long term physical problems. Try wearing thicker heels as opposed to stilettos to distribute weight more evenly across the feet. Always make sure you are wearing the proper shoes for the right occasion, such as sneakers for exercising. If you walk to work, try carrying your heels with you and changing into them once you arrive at work. Adding inserts to your heels can help cushion your feet and absorb shock. Full foot inserts or metatarsal pads are available.
If you have any questions please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Why High Heels Are Not Ideal for Healthy Feet
It is no secret that high heels are uncomfortable to wear for long periods of time. Although beauty is pain, you should not sacrifice the health of your feet for a stylish heel. Wearing high heels can potentially cause many different foot conditions that may be avoided by wearing proper footwear.
The structure of high heels forces weight of your body to get shifted forward toward the ball of the foot. The higher the heel you wear, the more weight and pressure get shifted forward. The pressure that your toes may experience from wearing heels may lead to hammer toes, bunions, and ingrown toenails. Extra weight and pressure resulting from wearing heels may cause stress fractures. Furthermore, heels may cause pinched nerves which may result in Morton’s neuroma.
High heels are even more dangerous for people who are clumsy. Falling or tripping while wearing heels can cause an ankle sprain or twist.
What many people don’t know is that heels can also cause back and knee problems. In order for your body to stay balanced on heels, your spine has to sway unnaturally, which adds stress to your spine muscles. This may cause you to experience a sore lower back.
If you decide to wear high heels regardless of the risks associated with them, there are ways you can minimize their harmful effects. One way to reduce injury is to massage and stretch your legs at the end of the day. Stretching can prevent the Achilles tendons and calf muscles from becoming too tight. If you are simply looking for more height, wedges and platforms provide a better surface area to distribute the body weight across compared to thinner heels.
If you experience pain from wearing high heels, it is important to see a podiatrist before any of your symptoms become worse.
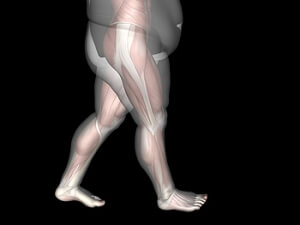
Weight and Gait

There is a growing concern regarding the prevalence of being overweight or obese among individuals aged 60 and older. Excess weight not only elevates the risk of chronic diseases but also poses a significant threat to physical performance in older adults, potentially leading to dependency. Being overweight or obese in later life is closely linked to adverse outcomes, including a higher risk of falls and an increased likelihood of developing walking limitations compared to those maintaining a normal weight. These challenges are compounded by factors such as low muscle strength, reduced cardiorespiratory capacity, and the elevated energy cost of walking. If you are older and overweight and it is impacting your mobility, it is suggested that you schedule an appointment with a podiatrist to discuss strategies that might help with improved functioning.
The more you weigh, the harder your feet must work to support your body. If you’re an obese individual and are concerned about your feet, contact Elie C. Daniel, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
People who are overweight are putting more pressure on their ankles, knees, and hips as well as their feet. This unfortunately can lead to variety of different issues.
Problems & Complications Stemming from Obesity
- When the body is overweight, it tries to compensate by changing the way that it moves. An obese person may lean forward and put extra weight on the wrong part of the foot. This puts unnecessary stress on the feet.
- Obese people are also more likely to develop type II diabetes which is a condition that causes a lot of foot problems. People with diabetes often don’t feel the cuts and sores that they may have on their feet, which can lead to more complicated and severe issues.
- Plantar fasciitis is another foot condition that can be caused by obesity. Plantar fasciitis is an inflammation of the tissue along the bottom of the foot, which causes pain and stiffness while walking and climbing stairs.
If you have any questions, please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Obesity and the Feet
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.
Surgery for a Broken Foot

When a foot bone fracture occurs, proper healing is critical for recovery. Treatment options vary based on factors, such as the fracture's severity and location. While some fractures can heal with casts, others necessitate more invasive approaches, like bone fracture repair, also known as open reduction and internal fixation, or ORIF, surgery. ORIF surgery is recommended when a broken bone cannot heal adequately with casting or splinting alone. This is often the case with compound fractures, where the bone breaks through the skin, or fractures involving joints, which can impact mobility. Recovery typically takes six to eight weeks, with initial pain, swelling, and numbness managed through painkillers, rest, and elevation. If you have broken your foot and it is a severe break or is not responding to customary conservative treatment measures, it is suggested that you schedule an appointment with a podiatrist to discuss whether surgery is an appropriate option for you.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Elie C. Daniel, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
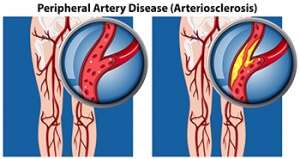
How Peripheral Artery Disease Affects the Feet
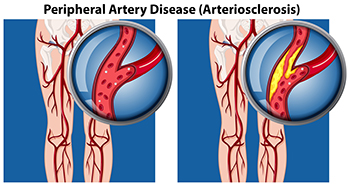
Peripheral artery disease, or PAD, is a condition akin to coronary artery disease and carotid artery disease. It affects arteries outside the heart and brain, particularly in the legs and feet. Peripheral artery disease involves the accumulation of fatty deposits on the inner linings of artery walls, narrowing the arteries and impeding blood flow. This reduction in blood circulation causes pain during activities such as walking, in addition to slow healing foot wounds, temperature disparities between feet, and potential development of gangrene. Severe cases may necessitate removal of the affected toe, foot, or leg. Individuals with diabetes face an elevated risk of PAD, which is further heightened by additional factors, including being overweight or obesity, physical inactivity, smoking, and high blood pressure. In addition, those with high LDL cholesterol, a family history of cardiovascular diseases, stroke, or a previous history of coronary artery disease or stroke are at higher risk of developing PAD. Early detection and intervention along with lifestyle changes, medication, and, in some instances, surgical procedures, can effectively manage PAD. If you have symptoms or risk factors of peripheral artery disease, it is suggested that you schedule an appointment with a podiatrist who is specially trained to manage this condition.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Elie C. Daniel, DPM from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Exploring Causes of Foot Pain

Foot pain, a common grievance that can significantly impede daily activities, can stem from various sources. One prevalent cause is improper footwear, as shoes that lack proper support or are too tight can lead to discomfort and pain. Overuse or strain, often the result of prolonged standing or excessive physical activity, can stress the muscles and joints in the feet. Conditions such as plantar fasciitis, characterized by inflammation of the tissue connecting the heel bone to the toes, contribute to persistent heel pain. Arthritis, affecting the joints, can also manifest as foot pain, particularly in the elderly. Additionally, injuries, nerve issues, or underlying medical conditions may contribute to discomfort. Identifying the root cause of foot pain is essential for targeted intervention. If you have any type of foot pain, it is strongly suggested that you consult a podiatrist who can determine the cause and offer appropriate treatment solutions.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Elie C. Daniel, DPM from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.