Connect With Us
Blog

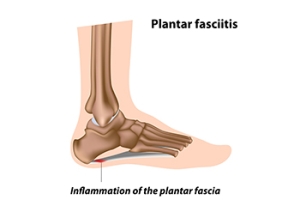
Plantar Fasciitis Is a Common Type of Heel Pain
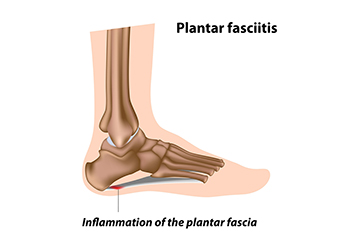
Because heel pain can be caused by several conditions, it is important to have it diagnosed correctly and treated properly. The most common form of heel pain is plantar fasciitis. This is an inflammatory condition of the plantar fascia, which is the long rubber band-like connective tissue that connects the front of the heel bone with the toes. The plantar fascia is on the bottom of the foot. It undergoes a great deal of stress and pressure while doing its duty of helping to form the arch, aiding in the propulsive phase of the walking cycle, and acting like a shock absorber of sorts. Excessive wear and tear and stretching of the plantar fasciitis can irritate it, inflame it, and even create micro-tears where it inserts at the heel bone. This is known as plantar fasciitis, a very painful form of heel pain. Plantar fasciitis can be brought on by certain sporting activities like running, being obese, standing for prolonged periods, and more. If you have heel pain that is at its worst in the morning when you take your first steps of the day, or after periods of rest, you may have plantar fasciitis. Consult with a podiatrist to have your heel pain diagnosed and treated.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Elie C. Daniel, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Can I Prevent Cracked Heels From Developing?

The foot condition known as cracked heels can be unsightly and uncomfortable. They develop as a result of having dry skin on the heels and surrounding area and may indicate a normal sign of aging. They can also come from wearing shoes with open backs like flip flops, which are popular shoes to wear in the warmer months. Additionally, they can come from standing on hard surfaces for most of the day or possibly from existing medical conditions. These can include eczema, psoriasis, or a thyroid disorder. In severe cases, the cracks in the skin may develop into fissures, which are deeper cracks that can bleed. Relief may come from washing and drying the feet daily followed by applying a good moisturizer. The feet will feel better when shoes that are worn have closed backs as well as wearing quality socks. Lastly, many patients have found it helps to drink fresh water frequently. If you have cracked heels and would like to know how to find relief and prevent them, please speak with a podiatrist.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Elie C. Daniel, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Symptoms of Sesamoiditis

There are many bones in your feet, and they each play an important role in helping your feet move and function. When important bones break or become inflamed, this can result in complications that might be painful or uncomfortable. For example, under your big toe are two sesamoid bones near the bottom of your feet. These bones can become inflamed from an injury or from tension that might occur if your big toe is suddenly and forcefully pushed upward. There are many different symptoms that can be felt from sesamoiditis. The most common symptom is pain. When putting pressure on the feet during walking or other physical activities, it is common for individuals with sesamoiditis to experience pain. However, what may make sesamoiditis difficult for the average person to identify is that there are not usually any noticeable, visual symptoms. That is to say that an individual might experience pain but not be able to point to any visual signs of sesamoiditis on their feet. To diagnose sesamoiditis, a medical professional can perform a bone scan or an MRI to identify the condition. If you are experiencing pain and inflammation in your sesamoid bones, contact a podiatrist who can help you treat the problem.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Elie C. Daniel, DPM of Illinois. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition that affects the joint that is just behind the big toe in the area known as the ball of the foot. It is most common in younger people and people who have just begun an exercise program. Since the sesamoid bones are like a pulley controlling the big toe, they can rub against each other and cause a gradual onset of pain. Pain may also be caused by the inflammation of tendons surrounding the bones. If ignored, sesamoiditis can lead to other, more serious problems such as severe irritation and fractures of the bones.
The cause of sesamoiditis is sudden increase in activity. The ball of your foot acts as a springboard to help you lift off when you are jogging or running. Sudden increase in the use of these bones or the tendon that controls them can cause irritation. The tendon then begins to develop inflammation and the joint begins to swell. People with smaller, bonier feet or those with a high arch are typically more susceptible to this condition.
Sesamoiditis is fairly simple to diagnose since the symptoms have a gradual onset rather than a sudden impact. The symptoms begin with slight irritation around the joint shortly after the increase in activity. The discomfort eventually turns to pain with light swelling and possibly redness. Although redness or bruising are rare, this may be a symptom. After each session of exercising, the aggravated joint becomes more irritated and increases into a very intense throbbing.
Treatment for sesamoiditis can vary depending on the severity of the situation. However, treatment is almost always approached in a noninvasive way. For a case that is just beginning the doctor may recommend a very strict rest period that will limit the activity allowed on the joint. If you must be active, a recommendation for as modified shoe or insole, along with bandaging and immobilizing the big toe will be made to ensure that pressure is not placed on the joint. For severe cases, it is typically recommended that the joint and the big toe be completely immobilized to allow adequate time to heal. Ice and an over the counter anti-inflammatory may can help with the pain and discomfort while you are at rest.
When you return to your regular exercise activities, it is recommended that you use an insole that will allow even distribution of impact to your entire foot, rather than just the balls of your foot. This will prevent further aggravation of the injury.
Arthritis Can Cause Pain in the Feet and Ankles
What Is Osteomyelitis?

Osteomyelitis is an infection and inflammation that can happen when a bacterial or fungal infection gets into a bone from the bloodstream or surrounding tissue. This condition can happen in the feet and can come on quickly or slowly and be severe or chronic. While it can occur at any age, older adults are more prone to osteomyelitis because they can experience health issues that increase their risk for infection that require surgery. Long bone infections, affecting arms and legs, are more common in children. Hematogenous osteomyelitis involves an infection to the bone from the bloodstream. It might enter the body through IV treatment. Non-hematogenous osteomyelitis can result from trauma, such as a fracture or open wound that requires surgery. Surgery that involves prosthetic materials, like metal pins, screws, or plates, can carry bacteria or fungi and cause this. Having diabetes or circulation problems can hamper treatment of this condition. Symptoms of osteomyelitis depend on the location of the infection, its severity, one’s age, and general health. Common symptoms include pain, swelling, fatigue, irritability, fever, chills, sweating, drainage, skin discoloration, and changes in walking. A delay in diagnosis and treatment can be serious, even fatal. Antibiotics or antifungal medication are usually administered to those with osteomyelitis. In some cases, surgery is needed to repair bone damage. If you have foot bone pain that is not related to a known issue, see a podiatrist immediately for an accurate diagnosis and swift, proper treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Elie C. Daniel, DPM from Illinois. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Princeton, Peru, and Mendota, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Congenital Foot Problems
A congenital foot problem is a problem affecting the feet, toes, and/or ankle that a child is born with. Several issues with a child’s feet can occur congenitally. Such problems include clubfoot, vertical talus, tarsal coalition, polydactyly, macrodactyly, and cleft foot. Some of these problems have a genetic basis, with someone in their family history having a gene causing the condition, and some are simply an anomaly.
The following are specifics about a few of these conditions:
- Clubfoot, also called congenital talipes equinovarus or talipes equinovarus, is When the tendons of the foot shorten, the bones are of an unusual shape, and the Achilles tendon is tight, causing an inward and downward pointing of the foot. The soles of the feet might also face each other. In most cases of clubfoot, both feet are affected. If not treated, the affected child will walk on the sides of their feet or ankles.
- Polydactyly is a condition where the child has more than five fingers or toes on either or both feet. Presentation usually consists of a nubbin or small lump of tissue without a bone, a toe that is partially formed but has no joints, or an extra toe.
- Vertical talus is where the talus bone forms in the wrong position, other bones in the foot do not line up properly, the front of the foot points up, and the bottom of the foot is stiff, has no arch, and usually curves out. This can occur in one or both feet and if left untreated, can lead to serious disability or discomfort as the child grows.
- Tarsal coalition is when there is an abnormal connection of two or more bones in the foot leading to severe, rigid flatfoot. The tarsal bones, located toward the back of the foot and in the heel, are the ones affected. This condition is often present at birth, but signs of the disorder usually come on in early adolescence.
- Cleft foot is a rare condition where the foot has missing toes, a V-shaped cleft, and other anatomical differences. Surgery can often help improve the foot’s function since the heel remains normal and is what is most needed for walking. The main issues with this affliction are whether the affected foot can fit into a shoe and the shape and appearance of the foot.
- Macrodactyly is when the toes are abnormally large due to overgrowth of the underlying bone or soft tissue. Having this condition makes it harder for the child to use the affected foot for certain activities.